Gingivitis vs. periodontitis: what's the difference?
Learn the key differences between gingivitis and periodontitis, their causes, symptoms, and effective treatment options.
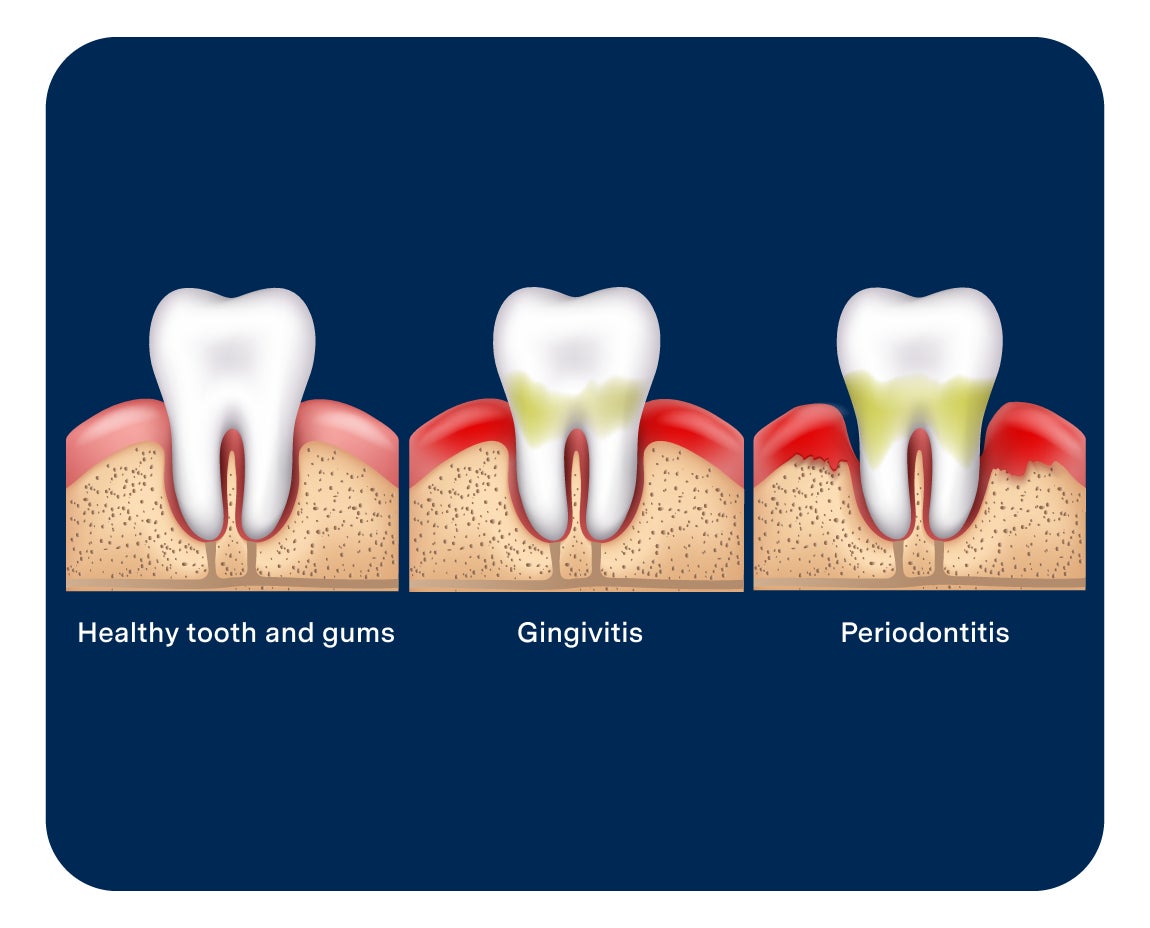
Gingivitis and periodontitis are both forms of gum disease, each a different stage. Gum disease starts as the more mild gingivitis and, when left untreated, proceeds to the more serious periodontitis. This article explains each type of gum disease in more detail, discusses how to spot them, and explores some ways to prevent both forms from developing or getting worse.
What is gingivitis?
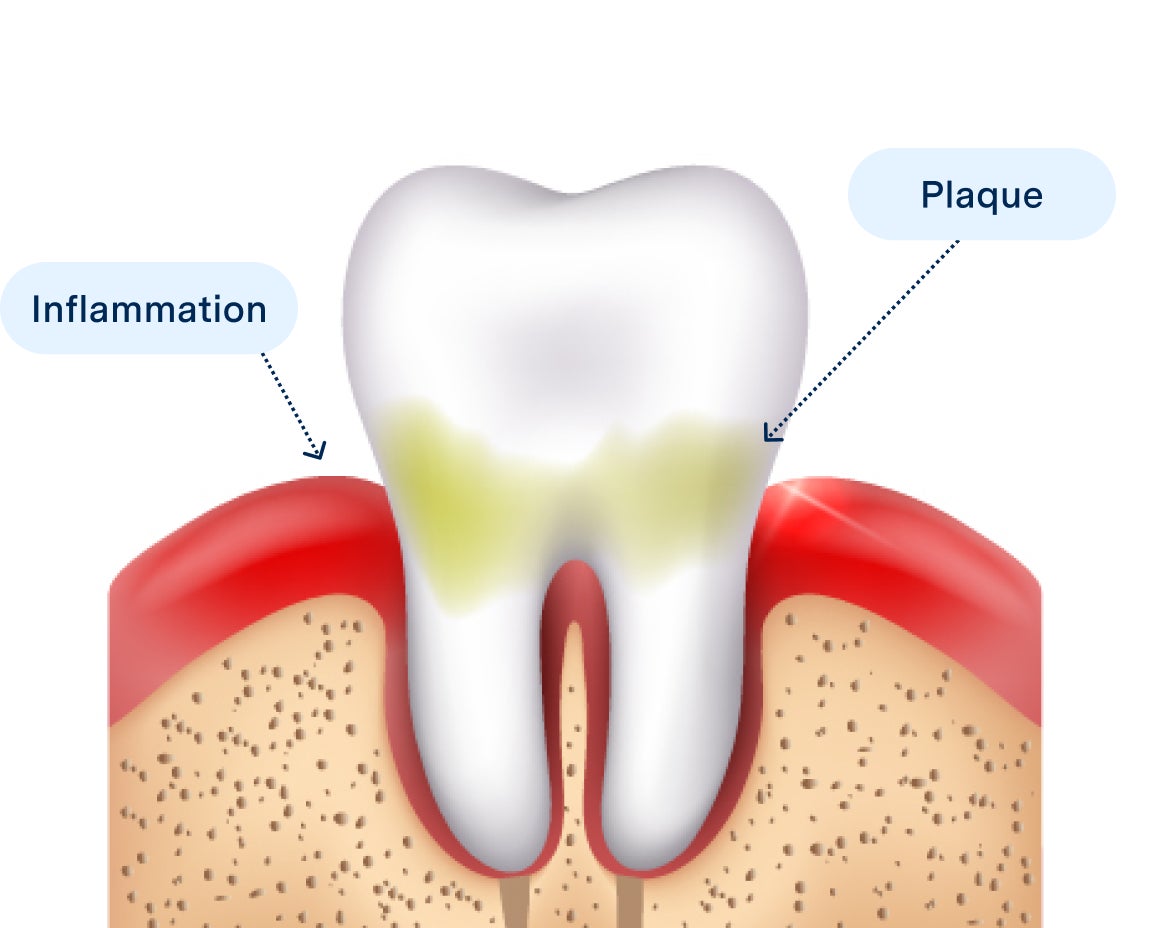
Gingivitis is the first stage of gum disease, a minor version caused by plaque that builds up on the portions of the teeth around the gum line. It can cause bleeding, irritation, and minor discomfort. It is the only form of gum disease that is curable and reversible when treated early by your dentist.
Signs of Gingivitis
Signs of gingivitis include:
Bleeding gums: Gums that bleed easily could indicate gingivitis.
Red or purple swollen gums: Gum infections can cause swelling and redness.
Sensitive gums: Gum disease can make gums painful or sensitive to touch, such as during brushing or dental cleanings.
Bad breath: Consistent bad breath, also called halitosis, can indicate bacteria buildup that may be causing gingivitis.
Unpleasant taste: Gingivitis can cause bad taste in the mouth due to plaque and bacterial buildup.
Gingivitis treatments
Here is how you and your dentist can treat gingivitis:

Oral hygiene habits: Brush twice daily, focusing on the gumline using a soft-bristled brush and gentle, circular motions. Floss and rinse once daily. When flossing, focus on removing plaque around the gumline. Rinse with an antimicrobial mouthwash.
Preventative cleanings: Attend your semi-annual routine cleanings with your dentist. They can address missed spots and remove tartar that brushing alone can’t remove.
Change in diet: Reduce sugar and alcohol consumption. Eat a balanced diet rich in vitamins and minerals to help your gums heal.
Quitting tobacco use: Tobacco products can accelerate gingivitis. Quitting tobacco can will benefit your overall oral health.
What is periodontitis?
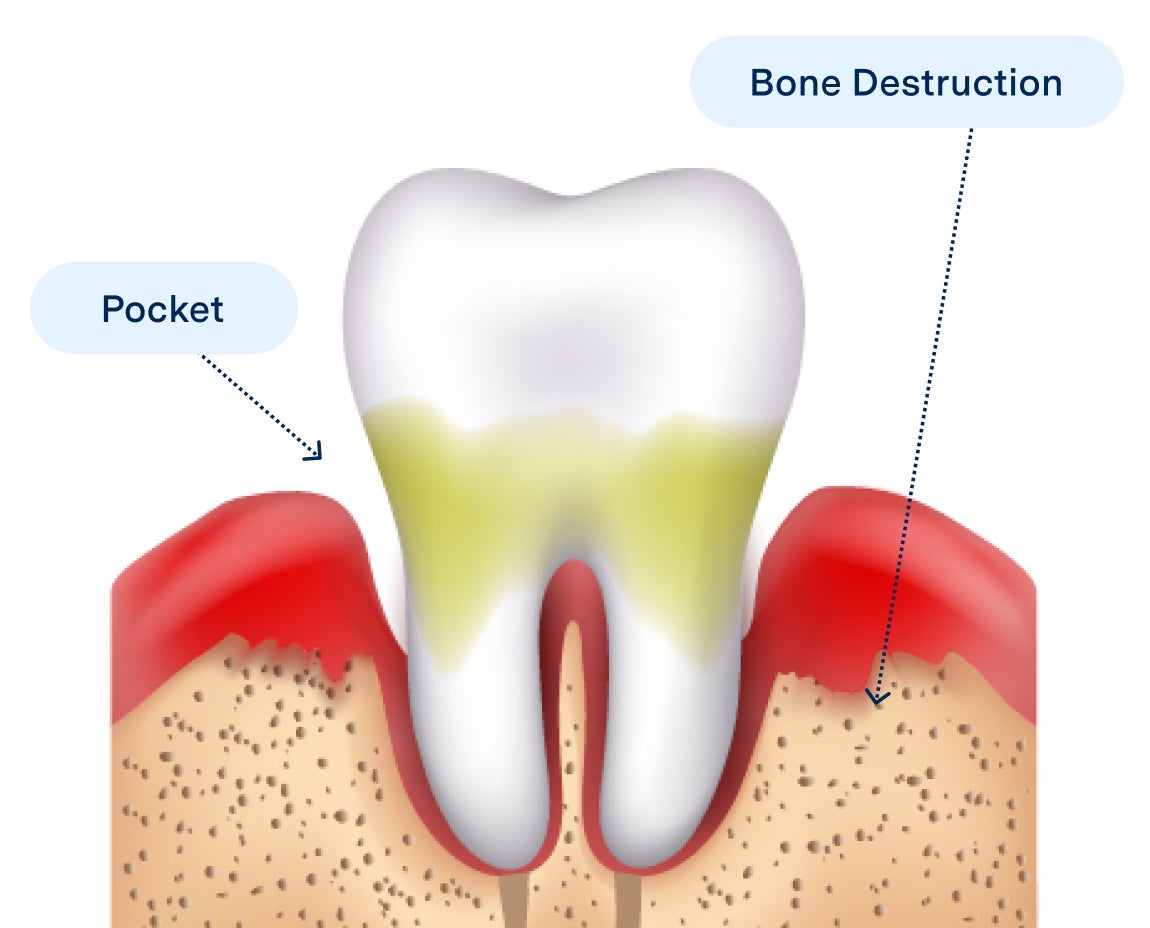
Periodontitis is a more advanced form of gum disease that happens when you don’t receive treatment to cure gingivitis. This form of gum disease spreads below the gumline, harming soft tissues and causing bone destruction. It can also cause gum recession, exposing the tooth roots underneath. As periodontitis progresses, it can lead to jawbone damage and loosen your teeth.
Signs of periodontitis
Signs of periodontitis include:
Red, swollen, or tender gums: A common symptom of periodontitis is inflamed gum tissue.
Bleeding when brushing teeth: Just as with gingivitis, gums that easily bleed can indicate periodontitis.
Loose or shifting teeth: The bone and tissue supporting your teeth can get damaged by periodontitis, causing them to loosen or shift.
Consistent bad breath, also called halitosis: Halitosis can indicate periodontitis in addition to gingivitis.
Pain when chewing: If you have periodontitis, you may experience pain or discomfort when chewing due to infection and inflammation.
Receding gums: Your gums may recede as a result of periodontitis, which can expose the tooth roots.
Pockets in gums: Periodontitis can lead to deep spaces in between your teeth and gums.
Periodontitis treatments
Here are some ways you and your dentist can treat periodontitis:

Scaling and root planing: This entails removing plaque and tarter under the gum line and on the root surfaces.
Antibiotics: These can kill bacteria and inhibit further growth.
Surgery: Sometimes surgical treatment is needed. Please speak with your dentist to figure out which the treatment is best for you.
Laser treatment: A minimally invasive procedure that kills bacteria.
Regular dental visits: Specialized cleanings, called periodontal maintenance, can help prevent periodontitis from progressing further and help manage the condition.
The cost of periodontal treatment is more than a routine cleaning since it;s the treatment of a disease, but dental insurance can often help with a significant amount of the cost. Additionally, Aspen Dental offers several ways to help make your treatments more affordable. We accept a variety of insurance plans, and also have dental financing and savings plan solutions that can meet your needs. Visit our Dental Financing and Insurance page to learn more.
Causes of gingivitis and periodontitis
The root causes of gingivitis and periodontitis are the same — a buildup of plaque and bacteria in the mouth. However, several factors can contribute to the development of these conditions:
Genetics and medical history: A family history of gum disease or similar issues could mean you have an increased risk of developing gum disease.
Poor oral hygiene: A lack of brushing, flossing, and rinsing allows bacteria and plaque to build.
Poor nutrition: Vitamin deficiencies could worsen gum health and facilitate gum disease.
Tobacco use: Tobacco use can weaken the immune system and reduce oxygen and nutrient flow to the gums, increasing the risk of gum disease.
Medication: Some medications may facilitate bacteria growth by reducing saliva and drying out the mouth.
Chronic conditions: Some conditions, like diabetes, can raise the risk of gum disease.
Hormonal shifts: Drastic hormonal shifts, such as those during puberty or pregnancy, could increase the risk of gum disease.
How to prevent gingivitis and periodontitis
Discipline and routine work can help you slow gum disease and, if it is still gingivitis, reverse it entirely. Here are some ways to do so:

Schedule regular dentist visits
Regular dental checkups allow your dentist to ensure your teeth and gums are thoroughly clean and help address any hard-to-reach spots. Dentists can also identify early signs of gum disease, giving you more time to stop it from progressing or even reverse it if it's gingivitis. Your dentist can provide personalized oral hygiene tips, such as improving flossing effectiveness, so your oral hygiene routine is more effective.
Maintain good oral hygiene
Good oral hygiene habits are your best defense against gingivitis and periodontitis:
Brushing: Brush twice daily with a soft-bristled toothbrush and fluoridated antimicrobial toothpaste. Use soft circular motions across the teeth and brush the gumline softly at an upward angle.
Flossing: Floss once daily, gently working the floss between each tooth to remove stickier debris from areas your brush can’t reach.
Rinsing: Rinse once daily with an antimicrobial mouthwash to clear any remaining debris out of your mouth and inhibit bacteria further. Swish vigorously for 30 to 60 seconds before spitting out.
Sticking to a consistent routine slows bacterial growth and keeps gum disease at bay.
Stick to a healthy diet
A healthy diet supplies your body with the nutrients it needs to fight bacteria and repair gum tissue. For example, Vitamin C is key for gum tissue repair, helping to heal wear and tear from eating. Antioxidants are helpful as well since these bolster the immune system. Limit sugary foods and alcohol since these can help feed bacteria or create dry mouth to accelerate growth. Be careful with hard or sharp foods that could damage the gums.
Avoid tobacco
Tobacco products reduce the flow of oxygen and nutrients to your gums. They also weaken your immune system. This combination helps bacteria grow and reduces the ability of your gums to fight infection. All forms of tobacco use can cause this, whether it's smoking, vaping, or chewing tobacco. Another benefit of quitting tobacco is reducing your risk of oral cancer, which can develop for similar reasons.
When to visit a dentist for gingivitis or periodontitis
Gum disease is a serious issue, even in its early stages as gingivitis. Once it progresses too far, it’s not reversible. If you notice symptoms like gum pain, bleeding when brushing and flossing, tenderness, swollenness, or gum recession, book an appointment with your dentist immediately. They can address the severity of the problem and promptly recommend the best action to fix it, whether curing gingivitis or stopping periodontitis from progressing.

Gingivitis vs. periodontitis FAQs
How does gingivitis progress to periodontitis?
Gingivitis progresses to periodontitis when the underlying bacteria and plaque causing the issue are not removed from the teeth and gums. Plaque and bacteria travel below the gumline, hardening into tartar and damaging bone and tissue. This also increases inflammation, swelling, bleeding, and pain in the gums.
How can you tell the difference between gingivitis and periodontitis?
The difference is generally in severity. Gingivitis can cause some pain, swelling, and bleeding, but it is not severe or permanent. Periodontitis also causes these symptoms but is more severe, and gum recession can occur. Advanced periodontitis can also loosen or shift teeth and create deep gum pockets.
Does periodontitis go away?
Periodontitis does not go away, unlike gingivitis, which can be reversed. However, you can stop the progression of periodontitis and manage the condition with excellent oral hygiene habits, regular dental visits, and scaling and root planing to fix the worst of the issue.
Get treatment for gingivitis or periodontitis
Gingivitis and periodontitis are two different stages of gum disease. Visiting the dentist regularly will ensure you receive the treatment you need. Additionally, early detection and proactive treatment can make a big difference and keep your gum disease from progressing. If you believe you have gum disease or are experiencing symptoms, you should visit the dentist right away. Schedule an appointment with Aspen Dental to get treatment for gingivitis or periodontitis and help protect your teeth.
